Advances in Neurointervention
By Julie Thompson

The neurointerventional team at Miami Valley Hospital knows how crucial it is to treat stroke and aneurysm victims rapidly with the most advanced tools. Recently, this group became the first in the area to acquire two new technologies to help patients stricken with the diseases.
Solitaire Revascularization Device
 A stroke occurs when blood flow to part of the brain is blocked by a blood clot forming in a brain artery. After a person experiences a stroke, every minute leads to the death of vital brain tissue.
A stroke occurs when blood flow to part of the brain is blocked by a blood clot forming in a brain artery. After a person experiences a stroke, every minute leads to the death of vital brain tissue.
However, the long-term outcome for victims may have improved thanks to the Solitaire device, which may be used up to eight hours after a stroke begins.
Solitaire, recently approved by the Federal Drug and Food Administration, is a minimally invasive technology, similar to a stent procedure for heart blockage. Physicians thread a thin catheter through an artery in the patient’s groin to the area of blockage in a brain artery. Within that catheter, they advance a miniature stent, a wire mesh tube that expands inside the artery. The stent opens in the blocked artery and blood flow is restored – even before the clot is fully removed.
The clot sticks to the stent after it is in place for about three minutes, and then the stent and the clot are pulled out. Neurointerventional specialist John Terry, MD, and his three colleagues have used the Solitaire device on a number of patients since acquiring the device in May. Its two biggest advantages, according to Dr. Terry, are it is fast and easy to use; and it restores blood flow almost immediately after being expanded in the artery.
Traditionally, there have been two ways to treat stroke victims: through the use of blood-clot-dissolving medication administered by vein; and by invasive interventional methods that utilize devices such as catheters.
However, both of those come with time limitations and risks. The blood-clot-dissolving drug known as a tissue plasminogen activator (tPA) can only be used in patients who arrive at the hospital within the first four and a half hours after the stroke symptoms begin.
And traditional interventional methods such as placing catheters in the arteries can be used up to about eight hours after the onset of a stroke. Such devices gradually break up the clot and remove it in pieces.
“When we used these interventional methods, we were not always certain we could re-establish blood flow; and when we did, it would sometimes take two to three hours,” Dr. Terry explains. “With Solitaire, we have been able to go from no blood flow to good blood flow within a matter of minutes.”
Over the years, the window of time for treating stroke victims has increased. “We know there is a point after which treatment is no longer effective, but we are trying to get as close to that line as possible. Solitaire helps us to do that,” says Dr. Terry.
Pipeline Embolization Device
A cerebral aneurysm is the abnormal enlargement or bulging of weak point in a brain’s blood-vessel wall. It most commonly causes harm by breaking and bleeding.
About every 18 minutes in the U.S., someone suffers a brain aneurysm, with nearly half of the episodes resulting in death. The new Pipeline embolization Device (PED) is a mesh tube that diverts blood flow away from the aneurysm.
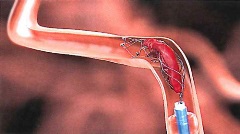
PED is used to treat adults age 22 or older with large or giant wide-necked intracranial aneurysms in the internal carotid artery, the major artery that supplies blood to the front of the brain. The metal device is placed through a catheter into the artery containing the aneurysm. The device covers the neck, or opening of the aneurysm, preventing it from being filled with blood.
PED redirects blood flow away from the aneurysm, causing the blood that remains in the aneurysm to clot, thereby preventing the aneurysm from rupturing. Once employed, the PED also reduces the outward push on the vessel’s walls, lessening the pressure on areas of the brain that might be compressed by a large aneurysm.
“An aneurysm is like a big balloon that will continue to press against something as long as it is filled up with pressurized blood,” Dr. Terry explains. “But if we can turn off the flow to that balloon, it will deflate, eliminating the pressure.”
The PED enables treatment of a wider group of people. Other techniques for treating wide-neck aneurysms could only be used on patients who were medically strong and who could undergo open (traditional) surgery. PED offers a minimally invasive option that delivers the same – if not better – result to the patient and usually results in a shorter hospital stay for the patient.
A Pivotal Time
Dr. Terry says, “This is an exciting time in my field of medicine with an influx of new devices emerging on the market – each one advancing the way in which brain diseases are treated.”
He notes that, “Over the past couple of years, Miami Valley has placed a high priority on a building a strong neurotinterventional team. One of the advantages of creating such a strong presence is that we can offer advanced technology to patients in the Dayton community.”

